Stuck at home, stuck in the mind
Students that contracted COVID-19 discuss their experiences and mental health
It is easy for us to let the pandemic we are living through overshadow how we care for not only our physical health, but also our mental health. For those who have contracted the virus, keeping a sound mind can be a challenge when clouded by external stressors.
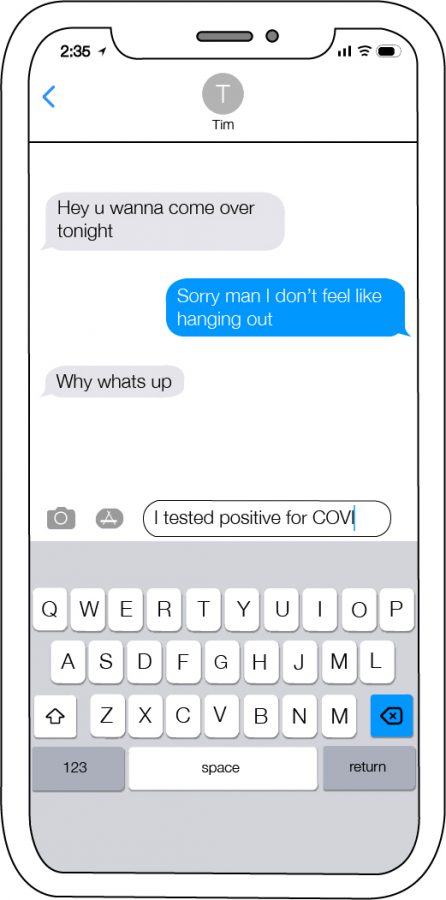
“My symptoms started after (working at) my job,” Peter Moreno, junior, said. “I went to get the test and came back positive. The doctor said I had it. It didn’t bother me, but it shocked me that I had the virus that made the whole world shut down.”
On March 17, the first case of COVID-19 was reported in Munster. Since then, various regulations were put into place to prevent the spread of the virus. Symptoms of the virus are similar to that of the flu, with an additional possible symptom of loss of taste or smell.
“Luckily I didn’t get it as bad since I was healthy and eating well before, and I only got minor symptoms,” Peter said. “The thing that started to get to me was that I couldn’t taste or smell. It just irritated me so much because I’m so used to eating anything healthy. Sometimes I lost my appetite and had to force myself to eat. It just kinda sucked. To this day, I don’t have my taste and smell 100% back anymore, which is kind of irritating.”
For Amaya Avila, freshman, who tested positive for the virus in November, dealing with the virus was a taxing experience.
“It was a bit draining,” Amaya said. “It made me a little sad when I had to sit in bed all day and not really do anything. I had headaches 24/7 so I couldn’t go on my phone either.”
In November, Indiana’s Governor Eric Holcomb announced that Indiana was halting the “Back on track” plan, where five stages marked the progression of the spread of the virus in the state. Alternatively, he announced that restrictions would be implemented on a county-by-county basis. As of three weeks ago, Lake County reached the highest possible “red” level. This level limits the social gatherings to 25 people.
“I felt really bad for my friends I was with because I had no symptoms the day before,” Amaya said. “I did hang out with my friends the day before (I found out), and I felt like I shouldn’t have done that. I mean you can’t really prevent it when you go to school with a bunch of people and hang out with your friends.”
 Since school shut down in the spring, many students struggled to cope with losing their social groups and habits. After weeks of social isolation, many ventured back into the real world, reconnecting with friends at a distance. While many were able to enjoy a slow return to former routines, others were still limited to the confines of their homes.
Since school shut down in the spring, many students struggled to cope with losing their social groups and habits. After weeks of social isolation, many ventured back into the real world, reconnecting with friends at a distance. While many were able to enjoy a slow return to former routines, others were still limited to the confines of their homes.
Savannah Frazier, senior, is one of millions across the country who are immunocompromised, a term meaning that one’s immune system is susceptible to disease or infection. In March, Savannah was diagnosed with Lupus, a chronic autoimmune disease, and has self-quarantined since her diagnosis.
“It’s been hard, I haven’t really been out too much,” Savannah said. “I kinda knew back when I was first diagnosed with Lupus that I’d have to be isolated and start making changes. I’m on the swim team, but I still feel pretty isolated from the rest of the people. (During) our season, I sit on the bleachers while everyone else is on deck waiting for their events. It’s been hard, but I’ve also grown used to it.”
The biggest challenge to preventing the spread of the virus is those who have disregarded the measures implemented for safety.
“The hardest part about it is seeing people that I’m close with, going out and about and doing stuff,” Savannah said. “Seeing people (disregard social distancing) upsets me because you know that there are other people out there doing worse than you, but you’re still not taking that into consideration as you go out there and do something. I can’t stop people, but I wish people could see things from my perspective.”
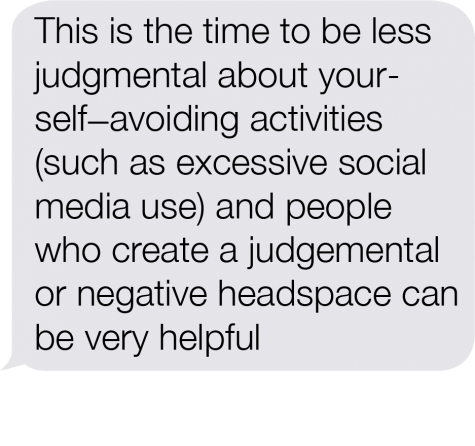
 The pandemic has made an impact on the mental well-being of many students, and created new barriers for individuals with preexisting mental health conditions. According to the American Psychological Association, social isolation has a negative effect on mental and physical health.
The pandemic has made an impact on the mental well-being of many students, and created new barriers for individuals with preexisting mental health conditions. According to the American Psychological Association, social isolation has a negative effect on mental and physical health.
“My mental health has been all over the place,” Savannah said. “I’ve had my downs but I’ve also had some days where I feel pretty good. At first it was sad not getting to see people. Other than that, I’d say for the most part I’m pretty okay. I also have a lot of good friends who I can talk to if I’m feeling really down about something.”
According to the CDC, symptoms of anxiety disorders and depressive disorders increased dramatically during the pandemic. This shift in a societal uneasiness was a result of a rapidly changing life
“I believe the biggest stressor for teens dealing with COVID is actually a two-way tie,” Mrs. Jennifer Dettlo, Spanish teacher, said. “First, the uncertainty of the pandemic affects all aspects of our daily lives. Since we know so little about the disease and how long we will have to deal with the effects of this pandemic, this creates too many unknowns. The end product is a generalized feeling of powerlessness. This is very debilitating.”
Uncertainty was a common theme throughout 2020, affecting social, political and emotional aspects of life.
“The isolation of adolescents can also be very damaging,” Mrs. Dettlo said. “Not having access to safe spaces, friends and support systems, not having access to normal social outlets and becoming even more reliant on social media and technology to create a sense of connection is really taking a toll on mental health. The adolescent population is exceptionally vulnerable to feeling displaced and marginalized during the most ‘normal’ of times; COVID-19 has amplified everyone’s feeling of being isolated from this normalcy.”
Many are familiar with the feeling of a “scare” – the dread that follows after learning that you might have been exposed, and thus could have been exposing others to the virus. In the same way, there is a lesser known feeling of guilt that hangs above a COVID-19 diagnosis.
“(There is) the guilt and shame that can accompany a positive (COVID-19) test result,” Mrs. Dettlo said. “Pressure generated by social media can paint a demonized version of who a COVID-19 patient may be.”
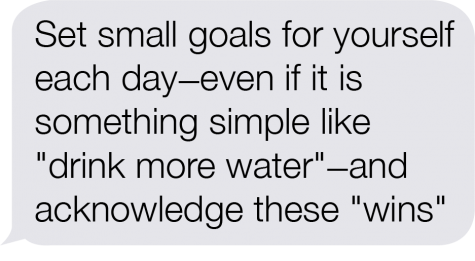
In the end, mental health needs to be taken more seriously. Taking care of psychological well-being is the quickest way to grow as a society.
“We should all tend to our mental health in the way we see our dentists and eye doctors and our GPs for yearly visits,” Mrs. Dettlo said. “The healthiest of people accept that this is simply part of being a human being and work to self-monitor and explore options for self care. The reality is we all have issues related to mental health that must be monitored and addressed; nobody is immune.”
Hi! My name is Lana, and I'm editor in chief this year! My hobbies include making frog rings, sending snail-mail to my friends, bullet journaling, photography,...